CAR-T therapy utilizes genetically modified T cells to express chimeric antigen receptors that specifically target tumor antigens on the cell surface, enabling precise recognition and killing of cancer cells. TCR-T therapy engineers T cells with transgenic T-cell receptors that recognize intracellular tumor antigens presented by major histocompatibility complex molecules, allowing for a broader range of cancer targets. Both therapies offer promising immunotherapeutic strategies but differ in antigen recognition mechanisms, with CAR-T excelling in hematologic malignancies and TCR-T showing potential in solid tumors.
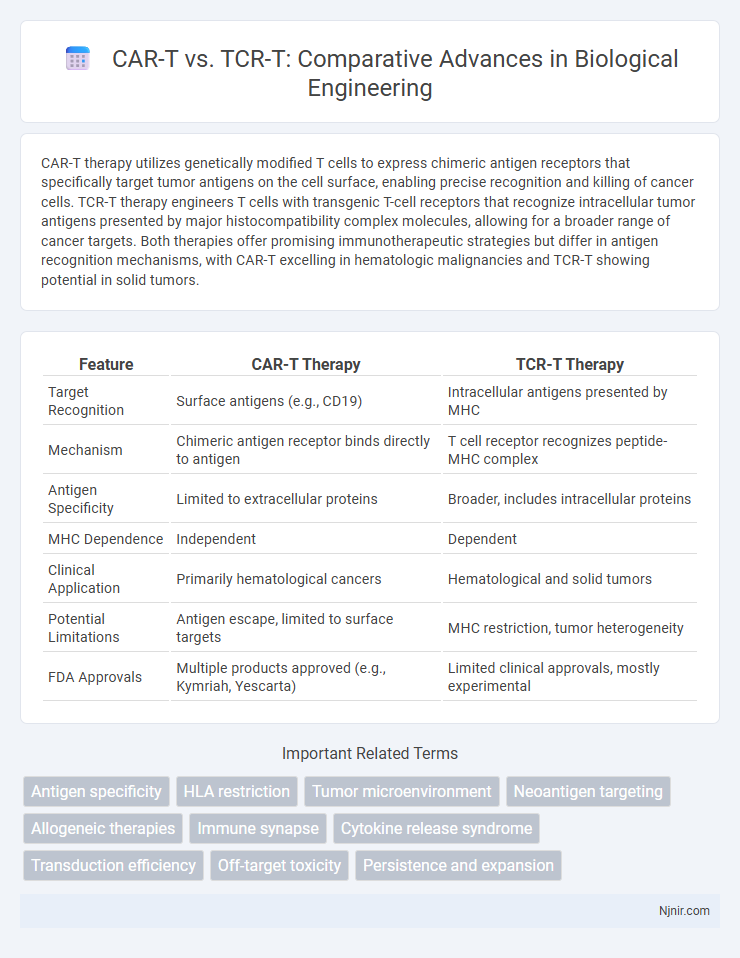
Table of Comparison
| Feature | CAR-T Therapy | TCR-T Therapy |
|---|---|---|
| Target Recognition | Surface antigens (e.g., CD19) | Intracellular antigens presented by MHC |
| Mechanism | Chimeric antigen receptor binds directly to antigen | T cell receptor recognizes peptide-MHC complex |
| Antigen Specificity | Limited to extracellular proteins | Broader, includes intracellular proteins |
| MHC Dependence | Independent | Dependent |
| Clinical Application | Primarily hematological cancers | Hematological and solid tumors |
| Potential Limitations | Antigen escape, limited to surface targets | MHC restriction, tumor heterogeneity |
| FDA Approvals | Multiple products approved (e.g., Kymriah, Yescarta) | Limited clinical approvals, mostly experimental |
Overview of CAR-T and TCR-T Therapies
CAR-T therapy utilizes chimeric antigen receptors engineered to target specific tumor antigens on the surface of cancer cells, enabling direct recognition and destruction by modified T cells. TCR-T therapy employs T-cell receptors engineered to recognize intracellular tumor antigens presented by major histocompatibility complex (MHC) molecules, allowing detection of a broader range of cancer targets. Both therapies represent advanced forms of adoptive cell transfer immunotherapy, but CAR-T is predominantly effective against hematologic malignancies, while TCR-T shows potential for solid tumors due to MHC-restricted antigen recognition.
Molecular Structures and Mechanisms
CAR-T cells incorporate chimeric antigen receptors with an extracellular single-chain variable fragment (scFv) for tumor antigen recognition, linked to intracellular signaling domains like CD3z and costimulatory molecules, enabling MHC-independent targeting. TCR-T cells utilize native T cell receptors recognizing peptide-MHC complexes, allowing detection of intracellular antigens but necessitating compatibility with the patient's HLA type. The molecular structure of CARs facilitates direct antigen binding, whereas TCRs rely on antigen processing and presentation, defining their distinct mechanisms in tumor cell eradication.
Antigen Recognition Specificity
CAR-T cells utilize engineered chimeric antigen receptors to recognize specific surface antigens independent of major histocompatibility complex (MHC), enabling direct targeting of tumor-associated proteins. TCR-T cells are designed with transgenic T-cell receptors that recognize peptide antigens presented by MHC molecules, offering the ability to target intracellular tumor antigens. The antigen recognition specificity of CAR-T is limited to extracellular epitopes, while TCR-T can target a broader range of antigens including those derived from intracellular proteins presented by MHC.
Therapeutic Applications in Oncology
CAR-T therapy targets surface antigens on tumor cells using engineered chimeric antigen receptors, showing high efficacy in hematologic malignancies such as B-cell acute lymphoblastic leukemia and non-Hodgkin lymphoma. TCR-T therapy recognizes intracellular tumor-associated antigens presented by MHC molecules, expanding treatment potential to solid tumors like melanoma and lung cancer. Both therapies demonstrate promising clinical outcomes, with CAR-T excelling in blood cancers and TCR-T offering broader applicability in solid tumor immunotherapy.
Manufacturing Processes and Engineering
CAR-T cell manufacturing involves transducing patient-derived T cells with a chimeric antigen receptor using viral vectors, requiring precise gene editing and expansion in bioreactors to ensure efficacy and safety. TCR-T cell production focuses on engineering T cells with specific T-cell receptors recognizing intracellular tumor antigens, demanding complex modification to maintain TCR pairing and avidity. Both platforms utilize sophisticated cell culture systems and quality control for scalability, but TCR-T manufacturing often faces additional challenges in optimizing TCR expression and avoiding mispairing compared to the more standardized CAR-T processes.
Clinical Efficacy: Successes and Challenges
CAR-T cell therapy has demonstrated remarkable clinical efficacy in treating hematologic malignancies, achieving high remission rates in conditions like acute lymphoblastic leukemia and certain lymphomas. TCR-T therapy shows promise in targeting solid tumors by recognizing intracellular antigens presented via MHC molecules, but faces challenges with antigen specificity and tumor heterogeneity. Both therapies encounter obstacles such as cytokine release syndrome, immune escape, and limited persistence, necessitating ongoing clinical optimization to enhance durable responses.
Safety Profiles and Adverse Effects
CAR-T and TCR-T therapies exhibit distinct safety profiles, with CAR-T often associated with cytokine release syndrome (CRS) and neurotoxicity due to its potent immune activation. TCR-T therapy, targeting intracellular antigens via T-cell receptors, generally shows lower incidence of CRS but poses risks of off-target effects and on-target off-tumor toxicity. Monitoring for hematologic toxicities and immune-related adverse events remains critical in both approaches to optimize patient safety and therapeutic outcomes.
Overcoming Tumor Microenvironment Barriers
CAR-T cells excel in targeting surface antigens but often struggle with the immunosuppressive tumor microenvironment (TME), limiting their efficacy in solid tumors. TCR-T cells recognize intracellular antigens presented by MHC molecules, enabling them to target a broader range of tumor antigens and potentially overcome TME resistance through enhanced infiltration and persistence. Advances in engineering both CAR-T and TCR-T cells, such as co-expression of cytokines or checkpoint inhibitors, aim to modulate the TME and improve antitumor responses.
Recent Advancements and Innovations
Recent advancements in CAR-T therapy have focused on enhancing specificity and reducing off-target effects through dual-targeting CAR designs and armored CARs incorporating cytokine support. Innovations in TCR-T therapy emphasize improved TCR affinity and diversity by leveraging neoantigen targeting and gene editing tools like CRISPR to overcome HLA restriction and tumor microenvironment immunosuppression. Both therapies benefit from advancements in manufacturing processes, enabling faster production and personalized treatments for hematologic malignancies and solid tumors.
Future Directions in Adoptive Cell Therapy
CAR-T and TCR-T therapies are advancing with innovations targeting solid tumors and improving antigen specificity. Emerging strategies include enhancing T cell persistence, reducing off-target effects, and integrating gene editing tools like CRISPR for precise receptor engineering. Future directions emphasize combining adoptive cell therapy with checkpoint inhibitors and personalized neoantigen targeting to overcome tumor heterogeneity and immune evasion.
Antigen specificity
CAR-T cells target surface antigens using chimeric antigen receptors, whereas TCR-T cells recognize intracellular antigen-derived peptides presented by MHC molecules, enabling broader antigen specificity.
HLA restriction
CAR-T cells recognize antigens independently of HLA molecules, while TCR-T cells require specific HLA-restricted antigen presentation for effective tumor targeting.
Tumor microenvironment
CAR-T cells face challenges penetrating the immunosuppressive tumor microenvironment, whereas TCR-T cells demonstrate enhanced tumor infiltration and responsiveness due to their recognition of intracellular tumor antigens presented by MHC molecules.
Neoantigen targeting
CAR-T cells primarily target surface antigens, whereas TCR-T cells enable precise recognition of intracellular neoantigens presented by MHC, making TCR-T more effective for neoantigen targeting in personalized cancer immunotherapy.
Allogeneic therapies
Allogeneic CAR-T therapies offer off-the-shelf solutions with broad tumor antigen targeting, while allogeneic TCR-T therapies provide enhanced specificity against intracellular antigens by leveraging native T-cell receptor recognition.
Immune synapse
CAR-T cells form a more rigid but less natural immune synapse compared to TCR-T cells, which create a dynamic and physiologically relevant synapse enhancing tumor antigen recognition and activation.
Cytokine release syndrome
CAR-T therapy induces more frequent and severe cytokine release syndrome compared to TCR-T due to its robust activation of immune effector cells targeting surface antigens.
Transduction efficiency
CAR-T cells typically exhibit higher transduction efficiency compared to TCR-T cells due to simpler vector integration and more robust gene expression mechanisms.
Off-target toxicity
CAR-T therapy exhibits off-target toxicity primarily due to antigen cross-reactivity and on-target off-tumor effects, whereas TCR-T therapy poses higher risks of off-target toxicity by cross-recognizing peptide-MHC complexes from unintended proteins, leading to potentially severe autoimmune-like responses.
Persistence and expansion
CAR-T cells demonstrate robust initial expansion but limited long-term persistence, whereas TCR-T cells exhibit enhanced persistence and sustained expansion due to their ability to recognize intracellular antigens presented by MHC molecules.
CAR-T vs TCR-T Infographic
 njnir.com
njnir.com