Photothermal therapy utilizes nanoparticles to convert light energy into heat, selectively destroying cancer cells with minimal damage to surrounding tissues. Photodynamic therapy relies on photosensitizers activated by specific wavelengths of light, producing reactive oxygen species that induce cell death. Both techniques offer targeted treatment options, but photothermal therapy provides rapid thermal ablation while photodynamic therapy triggers biochemical pathways for tumor destruction.
Table of Comparison
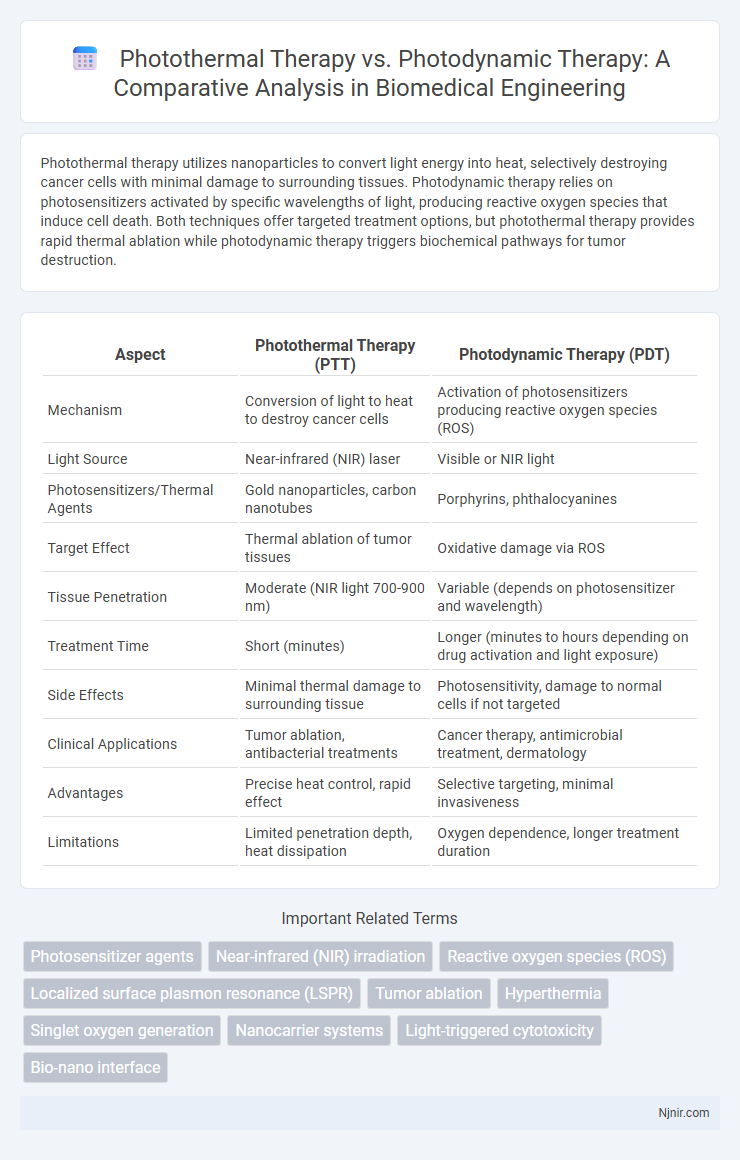
| Aspect | Photothermal Therapy (PTT) | Photodynamic Therapy (PDT) |
|---|---|---|
| Mechanism | Conversion of light to heat to destroy cancer cells | Activation of photosensitizers producing reactive oxygen species (ROS) |
| Light Source | Near-infrared (NIR) laser | Visible or NIR light |
| Photosensitizers/Thermal Agents | Gold nanoparticles, carbon nanotubes | Porphyrins, phthalocyanines |
| Target Effect | Thermal ablation of tumor tissues | Oxidative damage via ROS |
| Tissue Penetration | Moderate (NIR light 700-900 nm) | Variable (depends on photosensitizer and wavelength) |
| Treatment Time | Short (minutes) | Longer (minutes to hours depending on drug activation and light exposure) |
| Side Effects | Minimal thermal damage to surrounding tissue | Photosensitivity, damage to normal cells if not targeted |
| Clinical Applications | Tumor ablation, antibacterial treatments | Cancer therapy, antimicrobial treatment, dermatology |
| Advantages | Precise heat control, rapid effect | Selective targeting, minimal invasiveness |
| Limitations | Limited penetration depth, heat dissipation | Oxygen dependence, longer treatment duration |
Introduction to Photothermal and Photodynamic Therapies
Photothermal therapy utilizes near-infrared light to generate localized heat through photothermal agents, effectively destroying cancer cells by thermal ablation. Photodynamic therapy involves photosensitizers activated by specific light wavelengths, producing reactive oxygen species that induce cell apoptosis and necrosis. Both therapies offer minimally invasive options with targeted treatment for various cancers, leveraging different mechanisms of light-induced cytotoxicity.
Mechanisms of Action: PTT vs PDT
Photothermal Therapy (PTT) utilizes photothermal agents that convert near-infrared light into localized heat, inducing hyperthermia to selectively destroy cancer cells through protein denaturation and membrane disruption. Photodynamic Therapy (PDT) relies on photosensitizers activated by specific wavelengths of light to produce reactive oxygen species (ROS), primarily singlet oxygen, causing oxidative damage to cellular components and inducing apoptosis. While PTT's mechanism centers on thermal ablation, PDT's cytotoxic effect is driven by photoinduced oxidative stress targeting tumor tissues.
Key Biomaterials Used in PTT and PDT
Photothermal Therapy (PTT) primarily utilizes gold nanoparticles, carbon-based materials like graphene oxide, and copper sulfide nanoparticles due to their efficient light-to-heat conversion abilities. Photodynamic Therapy (PDT) relies on photosensitizers such as porphyrins, chlorins, and phthalocyanines that generate reactive oxygen species under light activation to induce cell death. Both therapies benefit from biocompatible and targeted delivery systems, including liposomes and polymeric nanoparticles, to enhance efficacy and minimize side effects.
Clinical Applications in Cancer Treatment
Photothermal therapy (PTT) uses near-infrared light to generate localized heat, inducing tumor cell apoptosis in cancers such as breast, lung, and melanoma, offering minimally invasive treatment with precise targeting. Photodynamic therapy (PDT) employs photosensitizers activated by specific light wavelengths to produce reactive oxygen species that selectively destroy cancer cells in head and neck, esophageal, and bladder cancers, enabling tumor-specific cytotoxicity with reduced side effects. Clinical trials demonstrate PTT's efficacy in reducing tumor volume and PDT's utility in managing superficial tumors, highlighting their complementary roles in integrative oncologic therapies.
Advantages and Limitations of Photothermal Therapy
Photothermal Therapy (PTT) offers precise tumor ablation by converting near-infrared light into heat, enabling deep tissue penetration and minimal damage to surrounding healthy cells. Its advantages include rapid treatment times and high spatial selectivity, though limitations involve potential overheating, incomplete tumor eradication due to heat diffusion, and the need for effective photothermal agents with strong biocompatibility. Unlike Photodynamic Therapy (PDT), which relies on reactive oxygen species and oxygen presence, PTT remains effective in hypoxic tumor environments but may face challenges in controlling thermal distribution and preventing collateral tissue damage.
Advantages and Limitations of Photodynamic Therapy
Photodynamic Therapy (PDT) utilizes photosensitizing agents activated by specific light wavelengths to produce reactive oxygen species that target and destroy cancer cells, offering high selectivity and minimal damage to surrounding healthy tissue. Advantages of PDT include its non-invasiveness, ability to treat localized tumors, and reduced systemic side effects compared to conventional therapies. Limitations involve light penetration depth restricting treatment to superficial or accessible tumors, potential skin photosensitivity post-treatment, and reliance on oxygen presence for effective reactive oxygen species generation.
Safety and Side Effects Comparison
Photothermal Therapy (PTT) primarily uses near-infrared light to generate localized heat, minimizing systemic toxicity and lowering risks of damage to surrounding healthy tissues. Photodynamic Therapy (PDT) involves photosensitizers activated by specific light wavelengths that produce reactive oxygen species, which may cause localized inflammation and photosensitivity reactions in some patients. Both therapies offer targeted cancer treatment options, but PTT generally exhibits fewer side effects due to its non-reactive heat mechanism compared to PDT's oxidative stress-induced cellular damage.
Recent Advances and Innovations
Recent advances in Photothermal Therapy (PTT) include the development of novel nanomaterials such as gold nanorods and carbon-based nanoparticles that enhance localized heat generation and improve tumor-targeting efficiency. Innovations in Photodynamic Therapy (PDT) focus on engineered photosensitizers with higher singlet oxygen yields and deeper tissue penetration, alongside the integration of oxygen-replenishing nanocarriers to overcome tumor hypoxia. Both therapies benefit from advances in combination treatments and smart delivery systems, increasing therapeutic efficacy while minimizing side effects.
Future Perspectives in Biomedical Engineering
Photothermal therapy (PTT) and photodynamic therapy (PDT) are advancing as transformative modalities in biomedical engineering, with future perspectives centered on enhancing treatment specificity and minimizing side effects through smart nanomaterials and targeted delivery systems. Integration of multiplexed imaging techniques and real-time monitoring is expected to refine dosage control and optimize therapeutic outcomes. Emerging research emphasizes the development of multifunctional nanoparticles capable of simultaneous diagnosis, therapy, and post-treatment assessment, driving personalized and precision medicine.
Conclusion: Choosing Between PTT and PDT
Photothermal therapy (PTT) harnesses heat generated by photothermal agents under near-infrared light to ablate tumors, offering rapid and localized treatment ideal for deep-seated cancers. Photodynamic therapy (PDT) relies on photosensitizers activated by specific light wavelengths to produce reactive oxygen species, effectively inducing cell death with minimal invasiveness but limited by oxygen availability and light penetration depth. Selection between PTT and PDT depends on tumor location, oxygenation status, and desired treatment precision, with PTT favored for hypoxic or deeper tumors and PDT preferred for superficial, well-oxygenated malignancies.
Photosensitizer agents
Photothermal therapy utilizes photosensitizer agents to convert light into heat for tumor ablation, whereas photodynamic therapy relies on photosensitizers to generate reactive oxygen species that induce cell death.
Near-infrared (NIR) irradiation
Near-infrared (NIR) irradiation in photothermal therapy enables targeted tumor ablation through localized heat generation, while in photodynamic therapy it activates photosensitizers to produce reactive oxygen species for cancer cell destruction.
Reactive oxygen species (ROS)
Photodynamic Therapy generates Reactive Oxygen Species (ROS) through light-activated photosensitizers to induce cytotoxicity, while Photothermal Therapy primarily relies on localized heat production with minimal ROS involvement for cancer cell destruction.
Localized surface plasmon resonance (LSPR)
Localized surface plasmon resonance (LSPR) enhances photothermal therapy by efficiently converting light to heat for targeted cancer cell ablation, whereas in photodynamic therapy, LSPR aids in generating reactive oxygen species to induce cytotoxicity.
Tumor ablation
Photothermal Therapy utilizes localized heat generated by photothermal agents under near-infrared light for efficient tumor ablation, whereas Photodynamic Therapy employs photosensitizers activated by specific light wavelengths to produce reactive oxygen species that induce tumor cell apoptosis and necrosis.
Hyperthermia
Photothermal Therapy utilizes targeted hyperthermia by converting light into heat to ablate tumors, while Photodynamic Therapy employs photosensitizers activated by light to generate reactive oxygen species without significant hyperthermia.
Singlet oxygen generation
Photodynamic Therapy generates singlet oxygen through photosensitizer activation to induce cytotoxic effects, while Photothermal Therapy primarily relies on localized heat production without singlet oxygen generation.
Nanocarrier systems
Nanocarrier systems enhance Photothermal Therapy by improving targeted heat delivery and Photodynamic Therapy by increasing photosensitizer stability and reactive oxygen species generation for cancer treatment.
Light-triggered cytotoxicity
Photothermal therapy induces cell death through localized heat generation using light-activated agents, whereas photodynamic therapy causes cytotoxicity by producing reactive oxygen species upon light activation of photosensitizers.
Bio-nano interface
Photothermal therapy leverages nanoscale materials to convert light into heat at the bio-nano interface for targeted cancer cell destruction, whereas photodynamic therapy utilizes photosensitizer-activated reactive oxygen species at this interface to induce tumor cell apoptosis.
Photothermal Therapy vs Photodynamic Therapy Infographic
 njnir.com
njnir.com