Endovascular stents provide durable support to occluded vessels, often made from metal alloys that ensure long-term patency but carry risks such as in-stent restenosis and chronic inflammation. Bioresorbable stents offer a temporary scaffold that gradually degrades, minimizing long-term complications and promoting natural vessel healing, although challenges remain in their mechanical strength and degradation rates. Advances in biomaterials and design optimization continue to enhance the safety and efficacy of bioresorbable stents, positioning them as a promising alternative to traditional metallic stents in vascular interventions.
Table of Comparison
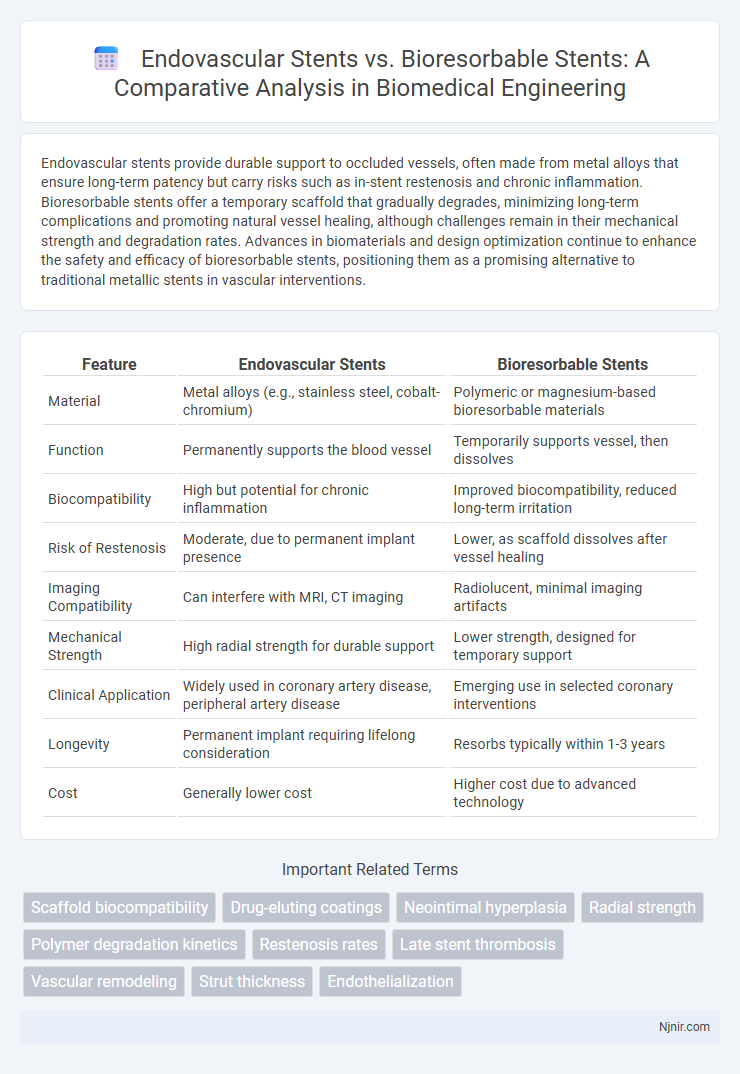
| Feature | Endovascular Stents | Bioresorbable Stents |
|---|---|---|
| Material | Metal alloys (e.g., stainless steel, cobalt-chromium) | Polymeric or magnesium-based bioresorbable materials |
| Function | Permanently supports the blood vessel | Temporarily supports vessel, then dissolves |
| Biocompatibility | High but potential for chronic inflammation | Improved biocompatibility, reduced long-term irritation |
| Risk of Restenosis | Moderate, due to permanent implant presence | Lower, as scaffold dissolves after vessel healing |
| Imaging Compatibility | Can interfere with MRI, CT imaging | Radiolucent, minimal imaging artifacts |
| Mechanical Strength | High radial strength for durable support | Lower strength, designed for temporary support |
| Clinical Application | Widely used in coronary artery disease, peripheral artery disease | Emerging use in selected coronary interventions |
| Longevity | Permanent implant requiring lifelong consideration | Resorbs typically within 1-3 years |
| Cost | Generally lower cost | Higher cost due to advanced technology |
Introduction to Endovascular and Bioresorbable Stents
Endovascular stents are small mesh tubes inserted into blood vessels to maintain vessel patency and prevent restenosis, typically made from metal alloys such as stainless steel or cobalt-chromium. Bioresorbable stents, composed of biodegradable polymers like polylactic acid, gradually dissolve within the body, reducing long-term complications associated with permanent implants. Recent clinical studies highlight the evolving role of bioresorbable stents in improving vascular healing while minimizing chronic inflammation compared to traditional endovascular stents.
Material Composition and Structural Differences
Endovascular stents are typically made from metal alloys such as stainless steel, cobalt-chromium, or nitinol, providing permanent vessel support with high radial strength and durability. Bioresorbable stents consist of polymer materials like polylactic acid (PLA) or magnesium-based alloys designed to gradually dissolve after vessel healing, minimizing long-term complications. Structurally, endovascular stents maintain a rigid scaffold indefinitely, whereas bioresorbable stents are engineered with controlled degradation profiles and flexible frameworks to accommodate vascular remodeling.
Mechanisms of Action: Traditional vs. Bioresorbable Stents
Endovascular stents mechanically support blood vessel walls by permanently implanting a metal scaffold to maintain vessel patency, while bioresorbable stents provide temporary scaffolding that gradually dissolves through hydrolysis, promoting natural vessel healing and reducing long-term complications. Traditional metal stents provoke a chronic inflammatory response and neointimal hyperplasia, potentially leading to restenosis, whereas bioresorbable stents aim to minimize this by releasing antiproliferative drugs and allowing restoration of vascular function post-degradation. The biodegradation timeline of bioresorbable stents varies based on polymer composition, typically spanning months to years, influencing both vessel remodeling and the risk profile compared to permanent metal counterparts.
Clinical Indications and Patient Selection
Endovascular stents are primarily indicated for patients with persistent arterial blockages and provide durable vessel support in cases of coronary artery disease or peripheral artery disease. Bioresorbable stents offer a temporary scaffold, ideal for younger patients or those with a higher risk of restenosis, as they gradually dissolve and reduce long-term complications. Patient selection hinges on factors such as lesion complexity, vessel size, and the need for long-term vessel patency, with bioresorbable stents favored when future interventions are anticipated.
Biocompatibility and Immunological Response
Endovascular stents, often made from metal alloys like cobalt-chromium or stainless steel, exhibit high mechanical strength but may provoke chronic inflammation and fibrotic tissue response due to permanent implantation. Bioresorbable stents, composed of polymers such as polylactic acid, offer improved biocompatibility by gradually degrading, which reduces long-term immunological reactions and facilitates natural vessel healing. Studies indicate bioresorbable stents minimize endothelial dysfunction and decrease immune cell adhesion compared to traditional metal stents.
Short-Term and Long-Term Efficacy Outcomes
Endovascular stents demonstrate immediate vessel patency with well-documented short-term efficacy through rapid arterial scaffolding and minimal recoil. Bioresorbable stents show promising long-term outcomes by gradually dissolving, reducing chronic inflammation, and restoring natural vasomotion, though their short-term complication rates may be higher. Comparative studies highlight endovascular stents' superiority in initial procedural success, while bioresorbable stents offer potential benefits in late lumen loss and avoidance of permanent implants over extended follow-up.
Complication Rates and Safety Concerns
Endovascular stents demonstrate lower early complication rates compared to bioresorbable stents, which are associated with higher incidences of thrombosis and vessel recoil. Bioresorbable stents offer the advantage of gradual polymer degradation, reducing long-term foreign body presence but raising safety concerns due to incomplete resorption and late scaffold collapse. Clinical studies highlight the necessity for vigilant monitoring of bioresorbable stent patients to mitigate risks of adverse cardiovascular events linked to device failure.
Advances in Stent Design and Coating Technologies
Endovascular stents have evolved significantly with the integration of drug-eluting coatings that reduce restenosis and enhance biocompatibility, while bioresorbable stents incorporate biodegradable polymers designed to provide temporary scaffolding and gradually dissolve, minimizing long-term complications. Advances in stent design emphasize thinner strut profiles and improved radial strength to optimize vessel support and reduce thrombogenicity. Novel coating technologies, such as polymer-free drug reservoirs and bioactive surfaces, further promote endothelialization and reduce inflammatory responses in both stent types.
Economic Impact and Healthcare Cost Analysis
Endovascular stents, predominantly made from metal alloys, have demonstrated long-term durability but often incur higher initial healthcare costs due to implantation and potential complications such as restenosis requiring repeat interventions. Bioresorbable stents, designed to dissolve within the body over time, may reduce long-term costs by minimizing chronic vessel irritation and the need for extended antiplatelet therapy, yet they currently involve higher production expenses and uncertain impacts on total healthcare economics due to limited long-term data. Comprehensive cost-effectiveness analyses reveal that while bioresorbable stents could lower indirect costs related to patient quality of life and future treatments, widespread adoption depends on further reduction in device costs and robust clinical evidence.
Future Directions in Biomedical Stent Development
Innovations in endovascular stents are increasingly focusing on bioresorbable materials that promote vascular healing while reducing long-term complications like in-stent restenosis and thrombosis. Future biomedical stent development emphasizes enhancing biocompatibility, drug elution profiles, and mechanical properties through advanced polymers and nanotechnology. Integration of smart stent systems with real-time monitoring capabilities represents a promising frontier to improve patient outcomes and personalized vascular therapies.
Scaffold biocompatibility
Endovascular stents provide permanent vessel support but may cause chronic inflammation due to metallic components, whereas bioresorbable stents offer temporary scaffolding with enhanced biocompatibility, reducing long-term immune response and promoting natural vessel healing.
Drug-eluting coatings
Drug-eluting coatings on endovascular stents provide controlled release of antiproliferative drugs to prevent restenosis, whereas bioresorbable stents with drug-eluting properties gradually dissolve, reducing long-term vascular complications while maintaining vessel patency.
Neointimal hyperplasia
Endovascular stents typically cause more neointimal hyperplasia due to permanent vessel scaffolding, whereas bioresorbable stents reduce neointimal proliferation by gradually dissolving and restoring natural vessel function.
Radial strength
Endovascular stents typically offer higher radial strength compared to bioresorbable stents, making them more effective in maintaining vessel patency under mechanical stress.
Polymer degradation kinetics
Polymer degradation kinetics in bioresorbable stents, governed by hydrolysis and enzymatic reactions, significantly influence mechanical support duration compared to permanent metal endovascular stents.
Restenosis rates
Endovascular stents exhibit lower restenosis rates compared to bioresorbable stents, which currently face higher restenosis due to scaffold degradation and inflammatory responses.
Late stent thrombosis
Endovascular stents exhibit a higher incidence of late stent thrombosis compared to bioresorbable stents, which degrade over time and reduce long-term thrombotic risks.
Vascular remodeling
Endovascular stents provide immediate vascular support but may impede natural remodeling, whereas bioresorbable stents promote vascular remodeling by gradually dissolving and restoring vessel flexibility.
Strut thickness
Endovascular stents typically feature thicker struts ranging from 80 to 140 microns, while bioresorbable stents prioritize thinner struts around 100 microns or less to enhance vascular healing and reduce restenosis risk.
Endothelialization
Endovascular stents promote faster endothelialization compared to bioresorbable stents, resulting in improved vascular healing and reduced risk of thrombosis.
Endovascular stents vs Bioresorbable stents Infographic
 njnir.com
njnir.com