Exoskeletons provide external mechanical support and enhance mobility by augmenting the user's natural movements, making them ideal for rehabilitation and assistance in patients with muscle weakness. Endoprostheses are implanted devices that replace or restore the function of damaged biological structures, commonly used in joint replacements and bone repair. Both technologies significantly improve patient quality of life but differ in their integration with the body and functional applications.
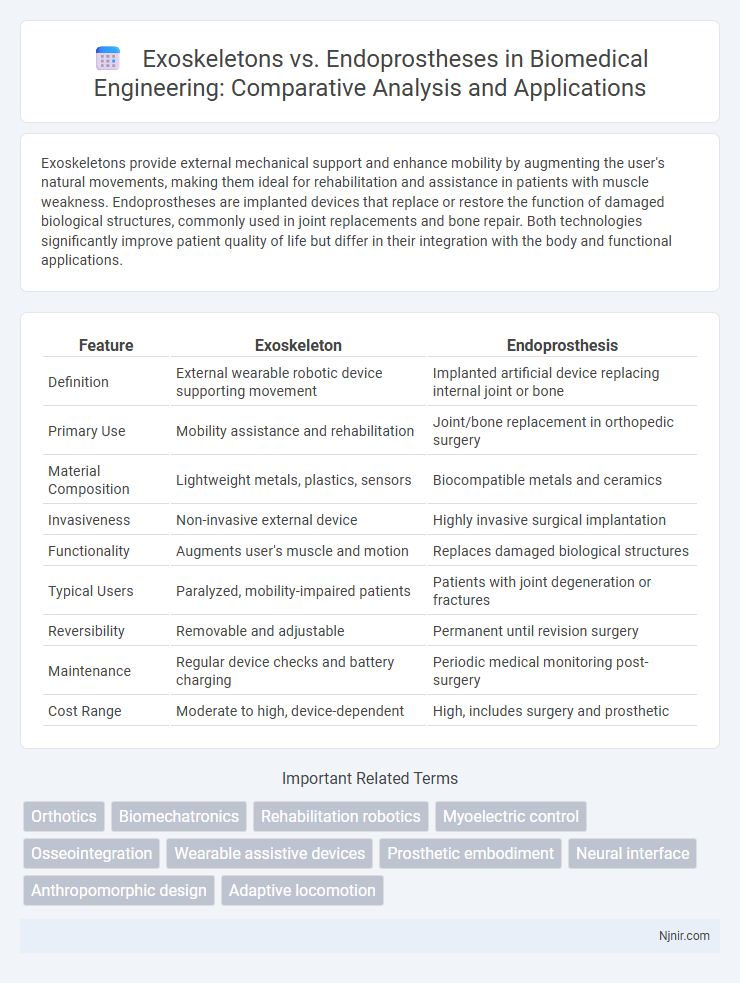
Table of Comparison
| Feature | Exoskeleton | Endoprosthesis |
|---|---|---|
| Definition | External wearable robotic device supporting movement | Implanted artificial device replacing internal joint or bone |
| Primary Use | Mobility assistance and rehabilitation | Joint/bone replacement in orthopedic surgery |
| Material Composition | Lightweight metals, plastics, sensors | Biocompatible metals and ceramics |
| Invasiveness | Non-invasive external device | Highly invasive surgical implantation |
| Functionality | Augments user's muscle and motion | Replaces damaged biological structures |
| Typical Users | Paralyzed, mobility-impaired patients | Patients with joint degeneration or fractures |
| Reversibility | Removable and adjustable | Permanent until revision surgery |
| Maintenance | Regular device checks and battery charging | Periodic medical monitoring post-surgery |
| Cost Range | Moderate to high, device-dependent | High, includes surgery and prosthetic |
Introduction to Exoskeletons and Endoprostheses
Exoskeletons are wearable robotic frameworks designed to support, enhance, or restore human movement by providing external mechanical assistance. Endoprostheses are implanted devices that replace or reconstruct damaged body parts, commonly used in orthopedic surgery to restore function internally. Both technologies play critical roles in rehabilitation and mobility enhancement but differ fundamentally in their integration with the human body and application methods.
Historical Evolution of Biomedical Assistive Devices
The historical evolution of biomedical assistive devices traces early exoskeleton concepts to ancient armor-like structures designed to enhance human strength, while endoprostheses emerged with the advent of internal limb replacements using metal alloys in the mid-20th century. Modern exoskeleton development accelerated with robotics and materials science breakthroughs in the 21st century, focusing on mobility augmentation and rehabilitation support. Advances in biocompatible materials and surgical techniques propelled endoprostheses to improve durability and integration with human tissue, shaping the trajectory of assistive technology innovation.
Design Principles: Exoskeletons vs Endoprostheses
Exoskeleton design principles center on external frameworks that support or enhance human movement, prioritizing modularity, adjustability, and load distribution to optimize user comfort and mobility. Endoprostheses focus on biomechanical integration within the body, emphasizing biocompatibility, precise anatomic fit, and durability to restore joint or limb function. While exoskeletons rely on external actuation and control systems for adaptive movement assistance, endoprostheses depend on material science and surgical techniques for stable, long-term implantation.
Materials and Technologies Used
Exoskeletons utilize lightweight, durable materials such as carbon fiber composites and aluminum alloys combined with advanced sensors, actuators, and microprocessors to enable enhanced mobility and support. Endoprostheses are crafted from biocompatible metals like titanium and cobalt-chromium alloys, often coated with hydroxyapatite to promote bone integration, and incorporate precision manufacturing technologies including 3D printing and CNC machining for custom-fit implants. Both leverage cutting-edge material science and engineering innovations to optimize functionality, durability, and patient outcomes in orthopedic and rehabilitation applications.
Clinical Applications and Use Cases
Exoskeletons provide external support and mobility assistance primarily in rehabilitation for spinal cord injuries and stroke patients, enabling improved gait training and muscle activation. Endoprostheses, implanted internally, are commonly used in joint replacement surgeries and limb salvage procedures for trauma or cancer patients, restoring structural integrity and function. Both technologies play crucial roles in enhancing patient outcomes, with exoskeletons focusing on functional recovery and endoprostheses emphasizing anatomical reconstruction.
Benefits and Limitations of Exoskeletons
Exoskeletons offer enhanced mobility and strength assistance for individuals with paralysis or muscle weakness, promoting rehabilitation and increased independence. Their limitations include high cost, limited battery life, and potential discomfort during prolonged use, restricting widespread adoption. Despite these challenges, exoskeletons provide real-time feedback and adaptability, differentiating them from endoprostheses which are surgically implanted and primarily focus on joint replacement or internal support.
Benefits and Limitations of Endoprostheses
Endoprostheses offer significant benefits such as improved joint function, pain relief, and enhanced mobility for patients with severe joint damage or deformities. Their integration into the body reduces external wear and tear while providing a more natural range of motion compared to external devices. Limitations include the potential for implant loosening, infection risks, and the finite lifespan of prosthetic materials, requiring possible revision surgeries.
Safety, Biocompatibility, and Patient Outcomes
Exoskeletons offer enhanced safety through external support and adjustable assistance, reducing fall risk and muscular strain in rehabilitation. Endoprostheses provide superior biocompatibility by integrating seamlessly with bone and tissue, minimizing immune response and implant rejection. Patient outcomes vary, with exoskeletons improving mobility and independence in acute phases, while endoprostheses deliver long-term functional restoration and stability in joint replacement scenarios.
Future Trends in Biomedical Engineering: Exoskeletons and Endoprostheses
Future trends in biomedical engineering emphasize the integration of smart materials and AI to enhance the functionality of exoskeletons, improving mobility and rehabilitation outcomes for patients with neurological disorders. Advances in biointerface technology and 3D printing are driving the development of more adaptive and personalized endoprostheses, optimizing prosthetic fit and sensory feedback. The convergence of robotics, neural engineering, and wearable sensors is set to revolutionize both exoskeleton and endoprosthesis designs, enabling seamless human-machine interaction and greater user autonomy.
Ethical, Social, and Regulatory Considerations
Exoskeletons present ethical challenges related to equitable access and potential socio-economic disparities, while endoprostheses raise concerns about long-term biocompatibility and bodily autonomy. Social acceptance of exoskeletons is influenced by perceptions of human enhancement, whereas endoprostheses often intersect with disability rights and identity issues. Regulatory frameworks must balance innovation and patient safety, with agencies like the FDA setting strict guidelines for clinical trials and post-market surveillance to monitor risks associated with both technologies.
Orthotics
Orthotic exoskeletons provide external support to enhance limb function, whereas endoprostheses involve internal implants replacing bone or joints to restore mobility.
Biomechatronics
Biomechatronics advancements enable exoskeletons to provide external mechanical support and enhance human mobility, whereas endoprostheses integrate internal biomechanical elements for joint and limb function restoration.
Rehabilitation robotics
Exoskeletons in rehabilitation robotics provide external support and mobility assistance for patients recovering motor function, while endoprostheses are implanted devices designed to restore or replace lost physiological functions internally.
Myoelectric control
Myoelectric control in exoskeletons enhances user mobility by detecting muscle signals for intuitive movement, while endoprosthesis uses implanted sensors for direct neural interfacing, offering more precise but invasive control.
Osseointegration
Osseointegration enables endoprostheses to directly anchor to bone, providing superior stability and natural load transfer compared to external exoskeletons.
Wearable assistive devices
Wearable assistive devices like exoskeletons provide external mechanical support to enhance mobility and strength, whereas endoprostheses are implanted internal devices designed to replace or augment biological structures.
Prosthetic embodiment
Prosthetic embodiment is enhanced in endoprostheses due to their integration with biological tissues, offering superior sensory feedback and natural movement compared to external exoskeletons.
Neural interface
Neural interfaces in exoskeletons enable direct brain-computer communication for enhanced motor control, whereas endoprostheses rely on implantable neural sensors to restore limb function through bioelectronic integration.
Anthropomorphic design
Anthropomorphic design in exoskeletons replicates natural human joint movements for external support, while endoprostheses integrate biomechanically within the body to restore internal joint function.
Adaptive locomotion
Exoskeletons enable adaptive locomotion by externally supporting and enhancing natural movement through real-time sensor feedback, whereas endoprostheses restore mobility internally by integrating with the neuromuscular system to facilitate biomechanical function.
Exoskeleton vs Endoprosthesis Infographic
 njnir.com
njnir.com