Smart bandages provide real-time monitoring and controlled drug delivery, enhancing wound healing through advanced sensors and responsive materials. Traditional wound dressings primarily offer basic protection and absorbency without the ability to track healing progress or release medication dynamically. Integration of smart technology in wound care reduces infection risk and accelerates recovery compared to conventional methods.
Table of Comparison
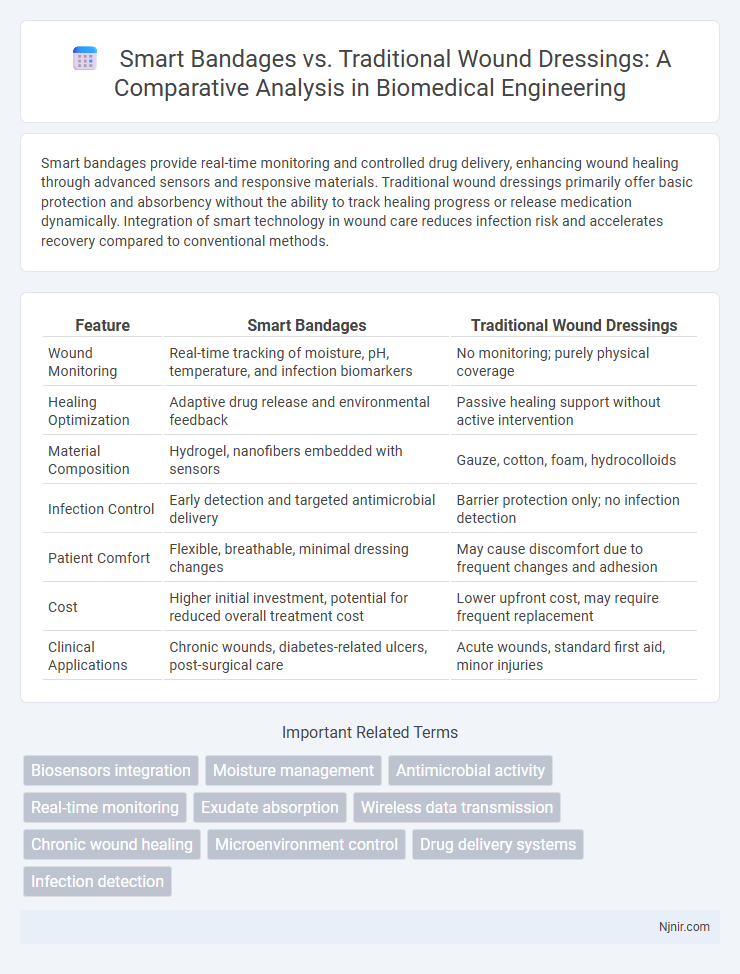
| Feature | Smart Bandages | Traditional Wound Dressings |
|---|---|---|
| Wound Monitoring | Real-time tracking of moisture, pH, temperature, and infection biomarkers | No monitoring; purely physical coverage |
| Healing Optimization | Adaptive drug release and environmental feedback | Passive healing support without active intervention |
| Material Composition | Hydrogel, nanofibers embedded with sensors | Gauze, cotton, foam, hydrocolloids |
| Infection Control | Early detection and targeted antimicrobial delivery | Barrier protection only; no infection detection |
| Patient Comfort | Flexible, breathable, minimal dressing changes | May cause discomfort due to frequent changes and adhesion |
| Cost | Higher initial investment, potential for reduced overall treatment cost | Lower upfront cost, may require frequent replacement |
| Clinical Applications | Chronic wounds, diabetes-related ulcers, post-surgical care | Acute wounds, standard first aid, minor injuries |
Introduction to Advanced Wound Care Technologies
Smart bandages represent a revolutionary advancement in wound care technology, integrating sensors and drug delivery systems to monitor healing and administer treatment in real time. Traditional wound dressings primarily provide passive protection and absorb exudate but lack the capability to actively respond to wound conditions. Advanced wound care technologies enhance healing outcomes by offering personalized, data-driven interventions that reduce infection risks and promote faster tissue regeneration.
Evolution of Wound Dressings: From Traditional to Smart
Traditional wound dressings, primarily composed of gauze and cotton, have long served as passive barriers that protect wounds but lack active healing capabilities. The evolution to smart bandages incorporates advanced materials embedded with sensors and drug delivery systems that monitor wound conditions such as moisture, pH, and temperature in real-time. These innovations enhance healing efficiency by providing targeted treatment and early infection detection, marking a significant advancement over conventional dressings.
Key Features of Traditional Wound Dressings
Traditional wound dressings primarily provide a physical barrier to protect wounds from contaminants and absorb exudate to maintain a moist healing environment. Materials such as gauze, cotton, and non-adherent pads are commonly used for their affordability and ease of application. These dressings require frequent changes and lack the ability to monitor wound conditions or deliver targeted therapy.
Innovations in Smart Bandage Design
Smart bandages integrate sensors that monitor wound conditions, such as pH, temperature, and moisture levels, enabling real-time data collection for optimized healing. These innovations include drug delivery systems that release antibiotics or growth factors precisely when needed, reducing infection risks and accelerating tissue regeneration. Advances in flexible electronics and biocompatible materials enhance patient comfort and ensure continuous wound assessment compared to traditional wound dressings.
Mechanisms of Action: Smart Bandages vs Traditional Dressings
Smart bandages incorporate sensors and drug delivery systems that monitor wound conditions such as pH, temperature, and moisture while providing targeted release of antibiotics or growth factors to accelerate healing. Traditional wound dressings primarily act as physical barriers to protect the wound from external contaminants and absorb exudate without sensing or responding to changes in the wound microenvironment. The advanced mechanisms of smart bandages enable real-time wound management and promote optimal tissue regeneration, contrasting with the passive and static function of conventional dressings.
Real-Time Monitoring and Data Integration in Smart Bandages
Smart bandages incorporate advanced sensors that enable real-time monitoring of wound conditions such as moisture levels, pH balance, and temperature, providing continuous data to healthcare providers. This integration allows for timely interventions and personalized treatment plans, reducing the risk of infection and accelerating healing compared to traditional wound dressings. Data collected from smart bandages can be transmitted wirelessly to electronic health records, facilitating seamless tracking and improved clinical decision-making.
Infection Control and Healing Efficiency
Smart bandages incorporate sensors and antimicrobial materials to continuously monitor wound conditions and deliver targeted treatment, significantly reducing infection risk compared to traditional wound dressings. Advanced materials in smart bandages facilitate faster healing by maintaining optimal moisture levels and enabling controlled drug release. Studies reveal that smart bandages improve healing efficiency and minimize complications, enhancing patient outcomes in wound management.
Patient Comfort and Compliance Considerations
Smart bandages enhance patient comfort by providing moisture regulation, temperature monitoring, and pain reduction through materials that adapt to wound conditions, reducing the need for frequent changes. Traditional wound dressings often cause discomfort due to adhesive irritation and lack of breathability, leading to increased risk of skin damage and decreased patient compliance. Improved compliance with smart bandages results from their ability to minimize dressing changes and offer real-time wound status feedback, promoting faster healing and patient satisfaction.
Cost Analysis and Accessibility of Wound Dressing Solutions
Smart bandages offer advanced wound monitoring capabilities, but their higher initial costs can limit accessibility compared to traditional wound dressings, which remain more affordable and widely available. Cost analysis reveals that while smart bandages may reduce long-term expenses through improved healing and fewer complications, traditional dressings provide cost-effective options for resource-limited settings. Accessibility challenges for smart bandages include the need for specialized technology and training, whereas traditional wound dressings benefit from established supply chains and ease of use.
Future Trends and Challenges in Wound Care Engineering
Smart bandages integrate biosensors and drug delivery systems for real-time monitoring and accelerated healing, surpassing traditional wound dressings in functionality. Future trends emphasize the development of multifunctional materials that promote tissue regeneration and enable wireless data transmission to healthcare providers. Challenges include ensuring biocompatibility, cost-effectiveness, and overcoming regulatory hurdles to facilitate widespread clinical adoption.
Biosensors integration
Smart bandages integrate advanced biosensors for real-time monitoring of wound conditions, enabling faster healing and personalized treatment compared to traditional wound dressings.
Moisture management
Smart bandages provide precise moisture management by continuously monitoring and adjusting wound hydration levels, whereas traditional wound dressings often rely on passive absorption without real-time feedback.
Antimicrobial activity
Smart bandages exhibit superior antimicrobial activity compared to traditional wound dressings by integrating sensors and controlled-release systems that actively detect and eliminate pathogens.
Real-time monitoring
Smart bandages provide real-time monitoring of wound conditions through integrated sensors, enhancing timely treatment compared to traditional wound dressings.
Exudate absorption
Smart bandages provide superior exudate absorption through advanced hydrogel and nanofiber materials compared to traditional wound dressings, enhancing moisture regulation and accelerating healing.
Wireless data transmission
Smart bandages enhance wound care by enabling wireless data transmission for real-time monitoring of healing conditions, surpassing traditional wound dressings that lack such connectivity.
Chronic wound healing
Smart bandages enhance chronic wound healing by providing real-time monitoring and controlled drug delivery, significantly improving treatment outcomes compared to traditional wound dressings.
Microenvironment control
Smart bandages precisely monitor and regulate the wound microenvironment by managing moisture, pH, and oxygen levels, significantly enhancing healing outcomes compared to traditional wound dressings.
Drug delivery systems
Smart bandages utilize advanced drug delivery systems with controlled, targeted release of medication, enhancing wound healing compared to traditional wound dressings that lack precise drug administration capabilities.
Infection detection
Smart bandages utilize embedded sensors for real-time infection detection in wounds, outperforming traditional wound dressings that lack automated monitoring capabilities.
Smart bandages vs Traditional wound dressings Infographic
 njnir.com
njnir.com