AI diagnostics in biomedical engineering enhances accuracy and speed by analyzing complex medical data beyond human cognitive limits. Machine learning algorithms continuously improve diagnostic precision through vast datasets, reducing human error and variability. However, integrating AI with human expertise ensures comprehensive evaluation, balancing computational efficiency with clinical intuition.
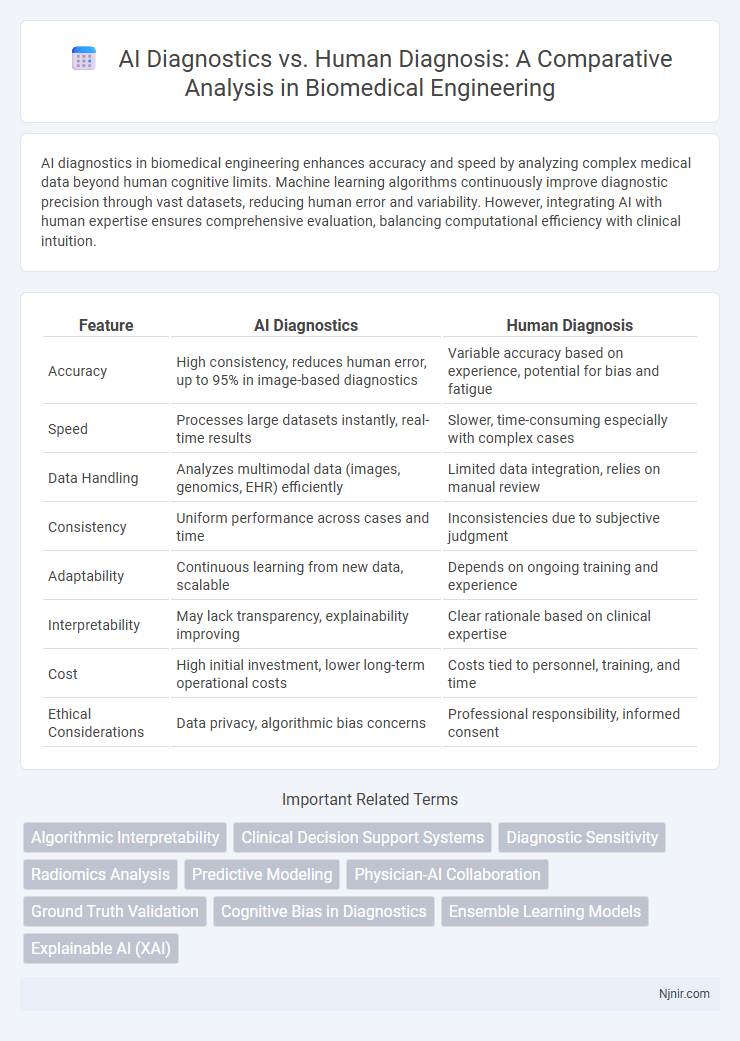
Table of Comparison
| Feature | AI Diagnostics | Human Diagnosis |
|---|---|---|
| Accuracy | High consistency, reduces human error, up to 95% in image-based diagnostics | Variable accuracy based on experience, potential for bias and fatigue |
| Speed | Processes large datasets instantly, real-time results | Slower, time-consuming especially with complex cases |
| Data Handling | Analyzes multimodal data (images, genomics, EHR) efficiently | Limited data integration, relies on manual review |
| Consistency | Uniform performance across cases and time | Inconsistencies due to subjective judgment |
| Adaptability | Continuous learning from new data, scalable | Depends on ongoing training and experience |
| Interpretability | May lack transparency, explainability improving | Clear rationale based on clinical expertise |
| Cost | High initial investment, lower long-term operational costs | Costs tied to personnel, training, and time |
| Ethical Considerations | Data privacy, algorithmic bias concerns | Professional responsibility, informed consent |
Introduction to AI Diagnostics in Biomedical Engineering
AI diagnostics in biomedical engineering utilize advanced machine learning algorithms and neural networks to analyze complex medical data, enhancing the accuracy and speed of disease detection compared to traditional human diagnosis. These technologies process vast datasets from imaging, genomics, and patient records to identify patterns that may be imperceptible to human clinicians. Integration of AI diagnostics in healthcare systems improves early detection, personalized treatment plans, and reduces diagnostic errors, driving a paradigm shift in modern medicine.
Evolution of Human Diagnosis: Strengths and Limitations
Human diagnosis has evolved through centuries of clinical observation, experiential knowledge, and pattern recognition, allowing physicians to integrate complex patient histories and contextual factors. Strengths include adaptability, empathy, and the ability to interpret ambiguous symptoms, while limitations involve cognitive biases, variability in expertise, and diagnostic errors. Despite advances, human diagnosis often struggles with processing large data volumes and detecting subtle patterns compared to AI-driven diagnostics.
How Artificial Intelligence Enhances Diagnostic Accuracy
Artificial Intelligence enhances diagnostic accuracy by analyzing vast datasets of medical images and patient records with greater speed and consistency than human capabilities. Machine learning algorithms continuously improve through pattern recognition, enabling earlier detection of diseases such as cancer, cardiovascular conditions, and neurological disorders. Integrating AI-driven tools in clinical workflows reduces human error, supports personalized treatment planning, and increases overall diagnostic confidence.
Comparative Analysis: AI vs Human Diagnostic Performance
AI diagnostics demonstrate higher accuracy rates, with machine learning models achieving up to 95% sensitivity in detecting conditions like cancer, outperforming average human diagnostic accuracy ranging from 70-85%. AI systems excel in processing vast datasets and identifying subtle patterns invisible to human clinicians, significantly reducing diagnostic errors and variability. However, human diagnosis benefits from contextual understanding and experiential judgment, which continue to play a critical role in complex or ambiguous cases where AI may struggle.
Data-Driven Decision Making: AI Algorithms vs Clinical Experience
AI diagnostics leverage vast datasets and advanced algorithms to identify patterns and predict outcomes with high accuracy, often surpassing human diagnostic speed. Clinical experience contributes nuanced understanding, context interpretation, and adaptability to complex cases where data may be limited or ambiguous. Combining AI's data-driven precision with clinicians' experiential insights enhances overall diagnostic accuracy and decision-making quality.
Speed and Efficiency in Diagnostic Procedures
AI diagnostics significantly reduce the time required for medical image analysis and pattern recognition, enabling faster identification of complex conditions compared to traditional human diagnosis. Machine learning algorithms process vast datasets instantaneously, enhancing diagnostic efficiency by minimizing errors and streamlining workflows in clinical settings. Rapid AI-driven diagnostics facilitate timely treatment decisions, improving patient outcomes and optimizing healthcare resource allocation.
Addressing Bias and Errors in AI and Human Diagnoses
AI diagnostics leverage vast datasets to identify patterns and reduce errors common in human diagnosis, yet they remain vulnerable to biases embedded in training data. Human diagnoses benefit from clinical experience and contextual understanding but can suffer from cognitive biases and inconsistent decision-making. Combining AI with human expertise enhances accuracy by addressing individual limitations, minimizing bias, and improving diagnostic outcomes.
Ethical Considerations: Trust and Accountability
AI diagnostics offer enhanced speed and accuracy in medical assessments but raise ethical concerns regarding trust and accountability. Unlike human diagnosis, where responsibility is clear, AI systems often operate as opaque "black boxes," complicating the attribution of accountability in case of errors. Ensuring transparency, robust validation, and clear guidelines for oversight is essential to foster patient trust and ethical integration of AI in healthcare.
Integration of AI Diagnostics into Clinical Practice
Integration of AI diagnostics into clinical practice enhances diagnostic accuracy by combining machine learning algorithms with clinician expertise. AI systems analyze vast medical data rapidly, identifying patterns that support early disease detection and personalized treatment plans. Emphasizing seamless collaboration between AI tools and healthcare professionals optimizes patient outcomes and operational efficiency within healthcare frameworks.
Future Perspectives: Collaboration between AI and Healthcare Professionals
The future of diagnostic accuracy lies in the synergy between AI diagnostics and human expertise, where AI algorithms analyze vast data sets at unprecedented speed while healthcare professionals provide contextual judgment and ethical oversight. Integration of AI-driven decision support systems into clinical workflows enhances early disease detection and personalized treatment planning by combining machine precision with human intuition. Collaborative models leveraging AI's predictive analytics alongside clinicians' experiential knowledge promise to revolutionize patient outcomes and streamline healthcare delivery.
Algorithmic Interpretability
Algorithmic interpretability in AI diagnostics enhances transparency and trust by enabling clinicians to understand and verify decision-making processes, unlike the often opaque reasoning in human diagnosis.
Clinical Decision Support Systems
Clinical Decision Support Systems in AI diagnostics enhance diagnostic accuracy and efficiency by providing real-time, data-driven insights that complement human clinical expertise.
Diagnostic Sensitivity
AI diagnostics demonstrate higher diagnostic sensitivity by accurately detecting subtle patterns and abnormalities that are often missed by human diagnosis.
Radiomics Analysis
Radiomics analysis in AI diagnostics significantly enhances tumor characterization accuracy and consistency compared to traditional human diagnosis by extracting quantitative imaging features beyond visual assessment.
Predictive Modeling
AI diagnostics leverage advanced predictive modeling algorithms that analyze vast datasets to identify patterns and forecast disease outcomes with higher accuracy and speed than traditional human diagnosis.
Physician-AI Collaboration
Physician-AI collaboration enhances diagnostic accuracy by combining AI's data-driven insights with physicians' clinical expertise to improve patient outcomes.
Ground Truth Validation
AI diagnostics demonstrate higher accuracy and consistency in ground truth validation compared to human diagnosis by leveraging large datasets and advanced algorithms.
Cognitive Bias in Diagnostics
AI diagnostics reduce cognitive bias in medical decision-making by processing vast data objectively, whereas human diagnosis is often influenced by subjective biases and limited cognitive capacity.
Ensemble Learning Models
Ensemble learning models in AI diagnostics combine multiple algorithms to enhance accuracy, outperforming traditional human diagnosis by reducing errors and improving disease detection rates.
Explainable AI (XAI)
Explainable AI (XAI) enhances AI diagnostics by providing transparent, interpretable insights that improve clinical decision-making and patient trust compared to traditional human diagnosis.
AI Diagnostics vs Human Diagnosis Infographic
 njnir.com
njnir.com