Wearable biosensors offer non-invasive, continuous monitoring of physiological parameters through external devices like smartwatches or patches, enhancing patient comfort and ease of use. Implantable biosensors provide more accurate and stable real-time data by being embedded directly within the body, enabling precise monitoring of critical biomarkers in complex environments. While wearables prioritize convenience and user-friendliness, implantables excel in long-term reliability and sensitivity for chronic disease management.
Table of Comparison
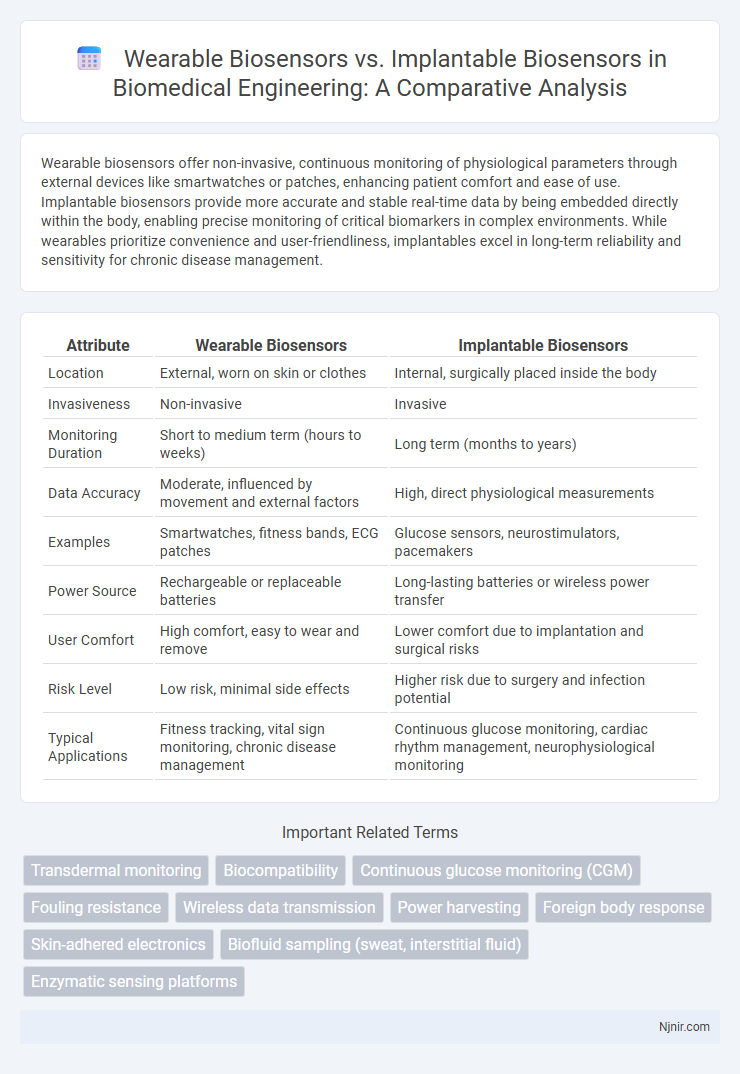
| Attribute | Wearable Biosensors | Implantable Biosensors |
|---|---|---|
| Location | External, worn on skin or clothes | Internal, surgically placed inside the body |
| Invasiveness | Non-invasive | Invasive |
| Monitoring Duration | Short to medium term (hours to weeks) | Long term (months to years) |
| Data Accuracy | Moderate, influenced by movement and external factors | High, direct physiological measurements |
| Examples | Smartwatches, fitness bands, ECG patches | Glucose sensors, neurostimulators, pacemakers |
| Power Source | Rechargeable or replaceable batteries | Long-lasting batteries or wireless power transfer |
| User Comfort | High comfort, easy to wear and remove | Lower comfort due to implantation and surgical risks |
| Risk Level | Low risk, minimal side effects | Higher risk due to surgery and infection potential |
| Typical Applications | Fitness tracking, vital sign monitoring, chronic disease management | Continuous glucose monitoring, cardiac rhythm management, neurophysiological monitoring |
Introduction to Wearable and Implantable Biosensors
Wearable biosensors monitor physiological signals through external devices attached to the skin, providing non-invasive, continuous health tracking for parameters such as heart rate, temperature, and glucose levels. Implantable biosensors are embedded within the body, offering highly accurate and localized monitoring by directly interacting with tissues or biological fluids, essential for chronic disease management and advanced diagnostics. Both technologies leverage biocompatible materials and miniaturized electronics, but implantable sensors require surgical procedures and rigorous biostability, contrasting with the ease and comfort of wearable devices.
Fundamental Principles of Biosensor Technology
Wearable biosensors operate on non-invasive signal acquisition techniques, primarily detecting physiological parameters such as heart rate, glucose levels, and sweat composition through surface electrodes and optical sensors. Implantable biosensors utilize biocompatible materials and microfabrication technologies to provide continuous, real-time monitoring of biomarkers within the body's internal environment, often leveraging electrochemical or enzymatic transduction mechanisms. Both types rely on transducer elements that convert biological responses into measurable electrical signals, but implantable sensors emphasize stability and integration with tissue for long-term accuracy, whereas wearable devices prioritize comfort and ease of use.
Design and Architecture: Wearable vs Implantable Devices
Wearable biosensors feature non-invasive designs with flexible materials and wireless communication modules tailored for continuous monitoring on the skin surface, emphasizing comfort and portability. Implantable biosensors require biocompatible materials, miniaturized architectures, and secure encapsulation to function accurately within the body while minimizing immune response and ensuring long-term stability. Both designs prioritize power efficiency and real-time data transmission, but implantable devices face stricter constraints on size, power source, and biostability compared to wearable devices.
Key Biomarkers and Analytes Detected
Wearable biosensors primarily detect biomarkers such as glucose, lactate, electrolytes, and cortisol through non-invasive sampling methods like sweat, interstitial fluid, or saliva. Implantable biosensors enable continuous monitoring of critical analytes including blood glucose, oxygen levels, and neurotransmitters directly within tissues or bloodstream, offering higher sensitivity and real-time data. Key biomarkers for implantable devices extend to cardiac markers and inflammatory cytokines, providing crucial insights for personalized medicine and chronic disease management.
Signal Acquisition and Data Transmission Methods
Wearable biosensors acquire signals non-invasively through surface electrodes or optical sensors, typically relying on Bluetooth Low Energy (BLE) or Wi-Fi for real-time data transmission to external devices. Implantable biosensors obtain signals directly from internal tissues or fluids via microelectrodes, often utilizing wireless telemetry or radio-frequency (RF) communication for continuous, secure data transfer. Both systems prioritize low power consumption and signal fidelity, but implantable biosensors require advanced biocompatible interfaces to maintain stable signal acquisition and data transmission within the body.
Biocompatibility and Patient Safety Considerations
Wearable biosensors offer non-invasive monitoring with minimal biocompatibility concerns, reducing the risk of skin irritation and allergic reactions, while implantable biosensors require advanced biocompatible materials like medical-grade silicones or titanium to prevent immune responses and tissue inflammation. Implantable devices pose higher patient safety risks, including infection, device migration, and the need for surgical implantation and removal, whereas wearable sensors minimize these issues through external application. The choice between wearable and implantable biosensors hinges on balancing continuous, accurate data acquisition against the complexity of ensuring long-term biocompatibility and patient safety.
Clinical Applications and Use Cases
Wearable biosensors offer non-invasive monitoring of vital signs such as heart rate, glucose levels, and physical activity, making them ideal for chronic disease management and real-time health tracking in outpatient settings. Implantable biosensors provide continuous, high-accuracy data for critical clinical applications like cardiac monitoring, drug delivery control, and detecting biomarkers for early disease diagnosis, often used in intensive care or long-term treatment scenarios. Both technologies enhance personalized medicine, but implantables deliver more precise internal physiological insights, whereas wearables prioritize user comfort and ease of use in daily life.
Challenges in Power Supply and Longevity
Wearable biosensors face challenges in power supply due to limited battery capacity and the need for frequent recharging, which affects continuous monitoring capabilities. Implantable biosensors require highly durable and biocompatible power sources to sustain long-term operation without causing tissue damage or requiring surgical replacement. Both types must balance energy efficiency and miniaturization to enhance longevity while maintaining reliable data transmission and sensor functionality.
Regulatory and Ethical Perspectives
Wearable biosensors face regulatory scrutiny primarily around data privacy, user consent, and device accuracy to ensure non-invasive safety standards, whereas implantable biosensors demand rigorous evaluation of biocompatibility, long-term stability, and surgical risks under stringent medical device regulations. Ethical challenges for wearable biosensors center on continuous monitoring consent and data security, while implantable biosensors raise concerns regarding autonomy, potential for unauthorized access, and implications of permanent bodily integration. Regulatory frameworks like FDA guidance emphasize differentiated approval pathways, reflecting the distinct risk profiles and ethical complexities inherent in each biosensor type.
Future Trends in Biosensor Innovation
Wearable biosensors continue evolving toward enhanced real-time health monitoring with advanced flexibility, energy efficiency, and integration of AI for predictive analytics. Implantable biosensors are advancing in miniaturization, biocompatibility, and wireless power, enabling continuous in vivo diagnostics and personalized drug delivery. Future trends emphasize hybrid systems combining wearable and implantable technologies for seamless, comprehensive health management and early disease detection.
Transdermal monitoring
Transdermal monitoring via wearable biosensors offers non-invasive, continuous measurement of physiological markers through the skin, whereas implantable biosensors provide direct, long-term biochemical data with higher sensitivity but require surgical insertion.
Biocompatibility
Wearable biosensors offer non-invasive monitoring with minimal biocompatibility concerns, while implantable biosensors require advanced biocompatible materials to prevent immune reactions and ensure long-term functionality.
Continuous glucose monitoring (CGM)
Wearable biosensors for continuous glucose monitoring (CGM) offer non-invasive, real-time glucose tracking through skin contact, while implantable biosensors provide long-term, highly accurate glucose measurement by being embedded under the skin, reducing calibration frequency and improving patient compliance.
Fouling resistance
Wearable biosensors offer moderate fouling resistance through surface coatings and periodic cleaning, whereas implantable biosensors require advanced anti-fouling materials and bioactive coatings to maintain long-term functionality within complex biological environments.
Wireless data transmission
Wearable biosensors utilize wireless data transmission through Bluetooth or Wi-Fi for continuous non-invasive monitoring, while implantable biosensors often rely on low-power radio frequency (RF) or near-field communication (NFC) to transmit critical physiological data securely from within the body.
Power harvesting
Wearable biosensors primarily rely on external power sources or intermittent energy harvesting from body heat and motion, while implantable biosensors utilize advanced energy harvesting techniques such as biofuel cells and inductive coupling to sustain continuous operation inside the body.
Foreign body response
Wearable biosensors minimize foreign body response by remaining external, while implantable biosensors induce a stronger foreign body response due to tissue integration and immune system activation.
Skin-adhered electronics
Skin-adhered wearable biosensors offer non-invasive, continuous health monitoring with flexibility and comfort, while implantable biosensors provide precise, long-term data within the body but require surgical insertion.
Biofluid sampling (sweat, interstitial fluid)
Wearable biosensors primarily sample sweat for non-invasive monitoring of biofluids, while implantable biosensors access interstitial fluid directly for more continuous and accurate biochemical analysis.
Enzymatic sensing platforms
Enzymatic sensing platforms in wearable biosensors offer non-invasive continuous monitoring with ease of use, while implantable biosensors provide higher accuracy and long-term stability by directly interfacing with target tissues.
Wearable biosensors vs Implantable biosensors Infographic
 njnir.com
njnir.com