Artificial organs offer customizable, synthetic replacements for failing biological systems, reducing the risk of immune rejection commonly seen in traditional transplants. Xenotransplantation involves transplanting organs or tissues from different species, which presents significant challenges due to potential cross-species disease transmission and immune compatibility issues. Advances in genetic engineering and immunosuppressive therapies are crucial to improving the safety and efficacy of xenotransplantation, while ongoing innovation in biomaterials enhances the functionality of artificial organs.
Table of Comparison
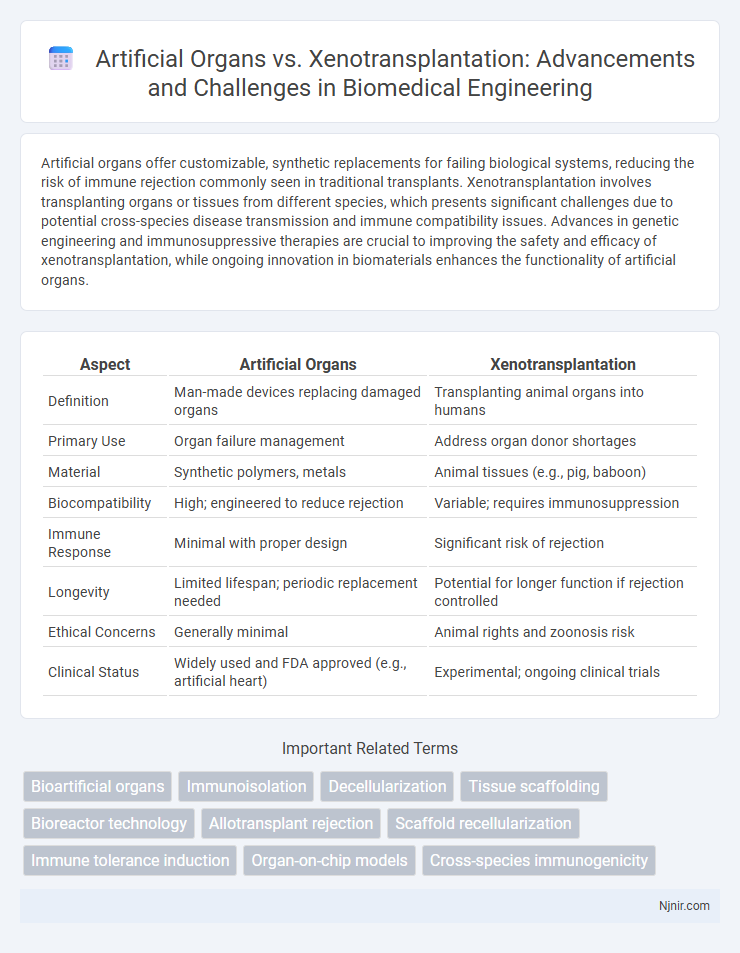
| Aspect | Artificial Organs | Xenotransplantation |
|---|---|---|
| Definition | Man-made devices replacing damaged organs | Transplanting animal organs into humans |
| Primary Use | Organ failure management | Address organ donor shortages |
| Material | Synthetic polymers, metals | Animal tissues (e.g., pig, baboon) |
| Biocompatibility | High; engineered to reduce rejection | Variable; requires immunosuppression |
| Immune Response | Minimal with proper design | Significant risk of rejection |
| Longevity | Limited lifespan; periodic replacement needed | Potential for longer function if rejection controlled |
| Ethical Concerns | Generally minimal | Animal rights and zoonosis risk |
| Clinical Status | Widely used and FDA approved (e.g., artificial heart) | Experimental; ongoing clinical trials |
Introduction to Artificial Organs and Xenotransplantation
Artificial organs replicate the function of damaged biological organs using biocompatible materials and advanced engineering techniques, often employed to bridge patients to transplantation or provide permanent organ replacement. Xenotransplantation involves transplanting organs or tissues from non-human animals, primarily pigs, into humans to address the shortage of donor organs and has seen significant progress with genetic modifications reducing immune rejection. Both approaches aim to alleviate organ failure but differ fundamentally in source and technology, impacting immunological compatibility and long-term viability.
Historical Development of Organ Replacement Technologies
The historical development of organ replacement technologies began with early artificial organs such as the first successful kidney dialysis machines in the 1940s, which laid the groundwork for mechanical organ support systems. Xenotransplantation research emerged in the 20th century, focusing on transplanting animal organs into humans to address donor shortages, with significant milestones including the use of baboon kidneys in human patients during the 1960s. Advances in immunosuppressive drugs and bioengineering have since accelerated both fields, driving innovations in biocompatible artificial organs and genetically modified animal organs for transplantation compatibility.
Mechanisms of Artificial Organs
Artificial organs function by replicating the physiological roles of natural organs through biomaterials, sensors, and electronic components that mimic biological processes. These devices, such as ventricular assist devices and bioengineered kidneys, utilize mechanical pumps, filtration systems, and biosensors to maintain homeostasis and organ-specific functions. Advances in tissue engineering and nanotechnology enhance the integration and functionality of artificial organs, improving biocompatibility and reducing immune rejection risks compared to xenotransplantation methods.
Principles and Processes of Xenotransplantation
Xenotransplantation involves the transplantation of living cells, tissues, or organs from one species to another, primarily using genetically modified pigs to overcome immunological barriers such as hyperacute rejection and zoonotic disease transmission. The process relies on precise genetic engineering to delete or modify specific pig genes, reducing antigenicity and improving compatibility with the human immune system while employing advanced immunosuppressive therapies to prevent graft failure. This approach contrasts with artificial organs, which are synthetic or bioengineered devices designed to replicate organ function without the complexities of cross-species immunological responses.
Biocompatibility and Immune Response Challenges
Artificial organs face significant biocompatibility challenges as materials must avoid triggering adverse immune responses, infections, or clotting while maintaining functionality over time. Xenotransplantation involves transplanting organs from non-human species, commonly pigs, which presents immune rejection risks due to species-specific antigens leading to hyperacute, acute, and chronic rejection without effective immunosuppression or genetic modification. Advances in biomaterials for artificial organs and gene-editing technologies like CRISPR to modify donor animal genomes aim to improve biocompatibility and reduce immune response challenges in both approaches.
Ethical Considerations in Artificial Organs and Xenotransplantation
Ethical considerations in artificial organs center on equitable access, long-term safety, and potential enhancement beyond natural human capabilities, raising debates about fairness and identity. Xenotransplantation ethics involve concerns about cross-species disease transmission, animal rights, and informed patient consent due to the experimental nature of using animal organs in humans. Both fields demand rigorous regulatory oversight to balance medical innovation with moral responsibility and public health.
Comparative Clinical Outcomes
Artificial organs offer consistent functionality with lower risk of immunologic rejection but face challenges such as mechanical failure and limited long-term durability. Xenotransplantation demonstrates potential for biological integration and continuous tissue regeneration, yet it carries significant risks of zoonotic infections and severe immune responses requiring lifelong immunosuppression. Comparative clinical outcomes highlight artificial organs providing more predictable immediate postoperative results, whereas xenotransplantation shows promise for long-term organ replacement contingent on overcoming immunological barriers.
Current Advancements and Technological Innovations
Recent advancements in artificial organs have leveraged biocompatible materials and 3D bioprinting techniques to create functional heart valves, kidneys, and lungs that reduce rejection risks and enhance patient outcomes. Xenotransplantation innovations focus on genetic modification of donor animals like pigs, using CRISPR technology to remove immunogenic markers and minimize organ rejection in human recipients. Both fields are increasingly integrating bioinformatics and immunomodulation strategies to improve graft survival rates and address organ shortages with scalable, effective solutions.
Regulatory and Safety Issues
Artificial organs face rigorous regulatory scrutiny to ensure biocompatibility, functionality, and long-term safety, with agencies like the FDA requiring extensive clinical trials and quality control standards. Xenotransplantation presents unique safety challenges due to the risk of cross-species viral transmission, prompting strict regulatory frameworks focusing on pathogen screening, immunosuppression protocols, and post-transplant monitoring to prevent zoonotic infections. Both fields must navigate evolving ethical considerations and public health safeguards to achieve regulatory approval and ensure patient safety in clinical applications.
Future Prospects in Organ Replacement Therapies
Artificial organs, driven by advancements in biocompatible materials and tissue engineering, offer promising long-term solutions for organ replacement with reduced immunological rejection. Xenotransplantation, leveraging genetically engineered animal organs, is progressing rapidly to address donor shortages but faces challenges in preventing cross-species disease transmission. Future prospects in organ replacement therapies likely involve integrating artificial organs with bioengineered tissues and enhanced xenotransplantation techniques to create safer, more effective treatment options.
Bioartificial organs
Bioartificial organs combine living cells and synthetic materials to enhance transplant success, offering a promising alternative to xenotransplantation by reducing immunological rejection and ethical concerns.
Immunoisolation
Immunoisolation techniques in artificial organs provide targeted immune protection by encapsulating cells to prevent rejection, whereas xenotransplantation relies on genetic modification and immunosuppressive strategies to overcome cross-species immune barriers.
Decellularization
Decellularization techniques enhance artificial organ development by removing cellular components to reduce immune rejection, offering a promising alternative to xenotransplantation in regenerative medicine.
Tissue scaffolding
Tissue scaffolding in artificial organs provides biodegradable frameworks promoting cell growth, whereas xenotransplantation relies on cross-species organ availability but faces immune rejection challenges.
Bioreactor technology
Bioreactor technology advances the development of artificial organs by providing controlled environments for cell growth, offering scalable and customizable alternatives to xenotransplantation that face immunological challenges.
Allotransplant rejection
Allotransplant rejection occurs when the recipient's immune system attacks transplanted human organs, making artificial organs and xenotransplantation critical alternatives to overcome immunological challenges.
Scaffold recellularization
Scaffold recellularization in artificial organs offers precise cellular integration and reduced immune rejection compared to xenotransplantation, enhancing long-term graft functionality and patient outcomes.
Immune tolerance induction
Immune tolerance induction in artificial organs involves bioengineered materials and immunomodulatory strategies, whereas xenotransplantation relies on gene editing and immune suppression to prevent rejection from cross-species immune responses.
Organ-on-chip models
Organ-on-chip models advance the development of artificial organs and improve xenotransplantation outcomes by simulating human physiology and immune responses at a microfluidic scale.
Cross-species immunogenicity
Cross-species immunogenicity in xenotransplantation presents significant immune rejection challenges that artificial organs can bypass by using bioengineered materials compatible with human biology.
Artificial organs vs Xenotransplantation Infographic
 njnir.com
njnir.com